Mike Islander
WKR
You do realize 1-1.3% is up to 60% greater risk than 0.8%?
Your numbers show that 3 is significantly different risk than 0 on CAC. He has been telling you the fact that someone has a 3 shows some calcification. The number of those people that then proceed to have CAD morbidity is real. Also, 10 year risk is short term when looking at a 30 or 40 year old man. We don’t know what that risk is in 30-40 years, but we can infer at simple extrapolation of 10 year risk that it’s 4-5%, and most would infer that it would be much higher than that. A relatively safe drug that has proven to reduce that risk is perfectly justifiable.
I want to be respectful, but I'm actually disappointed and a bit pissed off at your replies. Most charitably, you demonstrate why doctors sometimes recommend stuff based on a poor understanding of what numbers actually mean. It's a good demonstration of doubling down instead of admitting you were wrong. It's also a great demonstration of moving goalposts instead of just addressing my actual statements. Let's talk about where we disagree.
Absolute risk is what matters, not relative risk. It's five extra events per 1,000 people in 10 years (13 insead of 8). That's tiny! How about NNT? The NNT for CAC = 1-10 is 70-90. What is it for 0? 80-100. Almost meaningless difference.
EXAMPLE OF ABSOLUTE VERSUS RELATIVE RISK: If you have a 0.01% chance of dunking a basketball and I have a 0.02% chance, I’m technically 100% more likely to dunk on you. But in absolute terms, that’s just one extra dunk in ten thousand tries. Both of us are functionally not dunking that ball.”
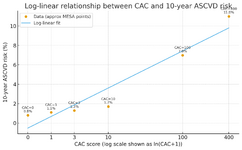
If you linearize the log of the CAC number, which is the curve that is used for MESA risk versus CAC, there are about 8 per 1000 individuals in 10 years for CAC = 0 and 13 per 1000 for CAC = 3. It's actually more of a hockey stick cuve around CAC = 10 or less, so it's even less risk than the straight line shows.
Your risk over time position is flawed. It's irresponsible to extrapolate 40 years out when you can actually measure the disease on demand. Every time you retake the CAC, the timeline RESETS. If I get a CAC = 3 in five years (or even a lower CAC, since a 3 is on the same level as noise in the CAC test), my 10 year risk starts all over again from that value. You seem to be (and correct me if I'm wrong) advocating for treating someone for decades based on a 30-40 year timeline. If not, I have no idea what you are talking about. Do you think everyone should just take statins and be done with it? That's not supported by the data, nor by a CAC = 3.
